As a caregiver or a loved one of a person living with dementia, you have likely run into the term "sundowning." You have come to the right place to expand your knowledge on what this is, how to manage it, and various tips for coping with sundowning.
What Is Sundowning?
Sundowning, commonly referred to as “sundown syndrome,” is a common symptom of dementia that affects a person's behaviour and mood and typically increases confusion as the day progresses towards the evening. It can be distressing for the person with dementia, their caregiver, and loved ones.
Sundowning is the name for the behaviours, feelings, and thoughts people living with dementia experience, as the name suggests, as the sun sets. While the behaviours often worsen around sunset or sundown, they can occur anytime during the day, not just at sunset. Sundowning symptoms often impact persons:
- Memory
- Thinking
- Personality changes
- Reasoning
- Behaviour
- Mood
Approximately 20% of people with dementia experience some of these sundowning behaviours at some point.
Sundowning behaviours range but can typically be described as restlessness, confusion, agitation, and irritability, and may lead to increased anxiety, pacing, yelling, and exhibiting aggressive behaviour.
It may also result in excessive pacing, rocking, wandering, following someone around, or crying hysterically.
People with dementia who experience sundowning may also experience sleep disturbances, including difficulty falling or staying asleep and increased fatigue during the day. The problems sadly get worse with sleep deprivation, including:
- Poor immune function and increased risk of infection
- Dehydration
- Delusions
- Physical illnesses
- Bodily pain
- Tiredness
Dementia sundowning happens between the middle and later stages of dementia, but it can occur at any stage of dementia. While sundowning may never go away completely, symptoms can be reduced and managed with appropriate care and support, and there are many management and treatment plans to consider.
Why Does Sundowning Occur?
While researchers are still investigating the exact cause of sundowning, many believe it results from the brain changes that occur with dementia, which can affect a person's ability to process and respond to sensory information.
Changes in light and environmental cues can also affect a person's sleep-wake cycle, leading to agitation and anxiety.
Significant disruptions in a person's internal body clock or circadian rhythm can trigger sundowning. The circadian rhythm regulates many biological processes and naturally changes with age. However, in people living with dementia, these changes can be more severe.
Specific triggers that bring on sundowning for people can include:
- Tiredness
- Hunger
- Thirst
- Medication side effects
- Changes in light
- Change in environmental cues
- Pain
- Being bored
- Hormonal disruptions
- Seasonal Affective Disorder
- General discomfort
- Feeling disoriented
- Changing the clocks
What Are The Early Signs Of Sundowning?
The early signs of sundowning vary for every person but are most commonly:
- Restlessness
- Agitation
- Confusion
- Irritability
- Increased anxiety as the evening approaches
- Difficulty falling or staying asleep
- Increased fatigue during the day
- Pacing
- Yelling
- Exhibiting aggressive behaviour
If you notice changes in your loved ones' behaviour, make sure to discuss these with your medical practitioner.
How To Deal With Sundowning
There are many approaches to dealing with sundowning that can help manage symptoms.
1. Create a soothing environment
Come the evening, focus on creating a tranquil and peaceful environment that can support reducing feelings of anxiety and agitation.
This can include dimming the lights, turning off any bright lights, including any tv shows, turning on soft, calming music, and minimising noise and distractions.
See our tips on how to find calm when living with dementia and our article on how to calm someone with dementia.
2. Develop a solid routine
A routine is helpful for someone with dementia as it can create structure and predictability. In the daytime, this can include a relaxing dementia-friendly activity, gentle exercises, reading, and outdoor walks. In the evening, we suggest a warm bath, shower, or reading or listening to a book to relax.
3. Avoid caffeine and sugar
Caffeine and sugary foods and drinks are not great for a solid night's sleep and may exacerbate symptoms of sundowning. Be sure to limit or avoid these drinks in the late afternoon. Read more here about the effects of caffeine on a person with dementia.
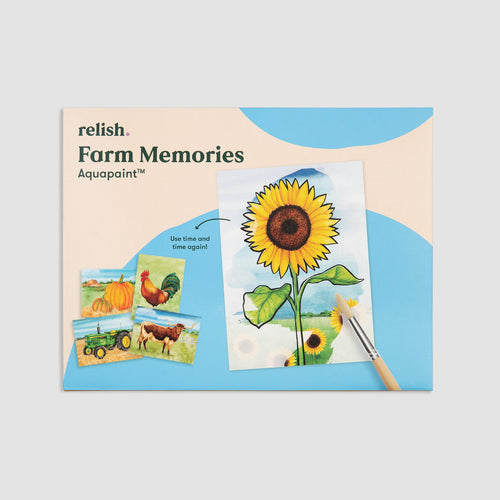
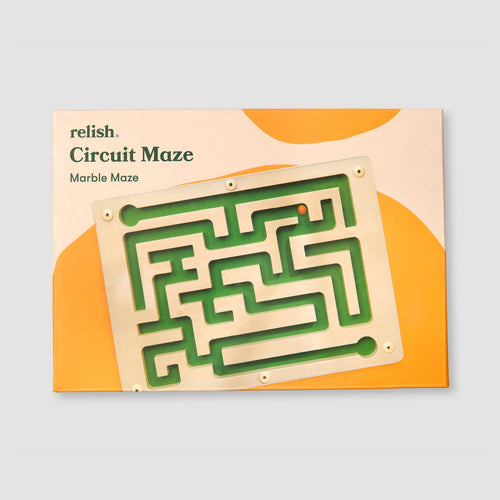
4. Redirect attention
If a person with sundowning is agitated or stressed, redirect their attention to something they love that comforts them, such as a favourite snack, drink, object, or activity.
See our list of activities to combat sundowning here.
5. Light Therapy
Therapy can be one of the most effective sundown dementia treatments.
Light therapy involves exposing the person with sundowning to bright light in the morning and early afternoon, which can help support their regulation of circadian rhythm and improve their sleep-wake cycle.
This therapy may reduce the severity of sundowning symptoms, such as agitation and confusion, and improve overall mood and behaviour.
You can carry out light therapy in several ways, such as using specialised light boxes or taking the person outside to get exposure to natural sunlight.
6. Involve relaxation techniques
Using relaxation techniques can be incredibly useful. Invite mindfulness and relaxation using deep breathing, muscle relaxation, or meditation. These activities are relatively easy to implore and can promote peace, reduce anxiety and agitation, and promote restful sleep. You might consider calming exercises such as hold & relax, which are gentle, sensory-based activities designed to support emotional wellbeing. For a broader range of calming approaches, explore our curated list of find calm activities, designed specifically for those living with dementia.
We’ve partnered with Breethe, a popular meditation and wellness app to bring you guided meditations and wellness tips. Sign up to our newsletter today and receive 20% off your Breethe Membership.
7. Get Moving in the AM
Encourage morning activities or appointments to establish a routine of stimulation and energy that can help promote regular sleep habits late in the day, as expelling energy is helpful to support the rest of the day.
Schedule more physically demanding activities during this time to ensure the person with dementia is engaged and active. Discourage napping during the day, as this can disrupt the sleep-wake cycle and make it more difficult for the person to fall asleep at night.
8. Use the Day Hub
The Day Hub is a dementia clock and routine organiser that supports people living with dementia. It includes the time, date, and states if it's morning, afternoon, evening, or night, helping those with dementia better orient themselves.
It is a helpful tool to remind people with memory loss to do certain activities, including eating, showering, taking medication, or winding down for bedtime.
It guides in independence and support for caregivers or loved ones so they know the person using the Day Hub is safe and can maintain their independence for as long as possible. You can learn more about it here!

How to prevent sundowning in dementia
Preventing sundowning is tricky, but plenty of strategies can reduce the frequency and severity.
These are:
- Ensuring sufficient sleep at night
- Avoid caffeinated beverages in the afternoon
- Limit alcohol
- Get outside in the sun - learn about how the great outdoors benefits those with dementia.
- Find joyful movement every day
- Take short naps if necessary but ensure that these naps are short and early on in the daytime
- Create a sense of structure
Is it possible to treat sundowning?
Research into sundowning in dementia has shown there is currently no cure at this time, but treating and managing symptoms is possible.
Personalised treatments are best to address specific needs. What works for one person in managing sundowning symptoms may not work for another. So, trying different preventative measures and seeing what works best is important. Dementia sundowning medication should only be used when prescribed by a healthcare professional.
Treatment can include both non-pharmacological and pharmacological interventions. It's important to note that treatment may need to be adjusted over time as the person's needs and symptoms change and that treatment aims to improve quality of life and reduce distress.
Typically, the tips above will support the treatment of sundowning. However, a doctor may prescribe medication in certain situations to help manage symptoms.
Medication for sundowning can come in many different forms, but the most common types of medication are:
- Antidepressants
- Antipsychotics
- Sleep aids, such as melatonin
A medical professional must prescribe, manage and monitor any medication taken.