Parkinson’s disease is a degenerative brain disorder which affects roughly 1 in 500 people in the UK. The typical age of onset is between 50 and 85 years old.
People living with Parkinson’s disease experience movement symptoms, like stiffness, tremors, and slowed motor functions. The condition is incurable but can be manageable. The symptoms of Parkinson’s worsen over time; most people with advanced-stage Parkinson’s disease need support with day-to-day activities.
Parkinson’s dementia is a common complication of Parkinson’s disease, characterised by a progressive decline in cognitive function. According to the Weill Institute for Neurosciences at the University of California, up to 80 percent of people with Parkinson’s disease will develop dementia. From the onset of motor symptoms, the average time it takes to develop dementia is around ten years.
This article will talk you through the symptoms of Parkinson’s disease dementia, alongside causes, diagnostic practices and available treatments.
What are the symptoms of Parkinson’s disease dementia?
The symptoms associated with Parkinson’s disease dementia vary. They will change and worsen as the condition progresses. Below are some of the most common symptoms according to the different Parkinson’s dementia stages.
Early symptoms
The symptoms of Parkinson’s dementia begin with minor cognitive changes, known as mild cognitive impairment (MCI). MCI typically develops around five years after movement symptoms have started - though this varies from person to person.
The symptoms of MCI may initially be very subtle. Many people experience:
- Increased forgetfulness
- Loss of train of thought mid-speech or activity
- Difficulty finding their way around familiar places
- Increased impulsivity/poorer judgement
It’s also not uncommon for people to develop mental health issues, like depression or anxiety, alongside MCI.
Symptoms of Parkinson’s disease dementia
As MCI advances, a person living with Parkinson’s may ultimately be diagnosed with Parkinson’s disease dementia. Dementia symptoms vary from person to person but often include the following:
- Communication difficulties: Difficulty finding the right words, forgetting names for objects, trouble recalling people’s names, increased misinterpretation of what other people say
- Speech problems: Louder or quieter than usual speech, difficulty forming words smoothly
- Short and long-term memory loss: Forgetting appointments and recent conversations, misplacing objects, getting lost in familiar places, confusion of life history (e.g. forgetting a particular family member is married or has passed away)
- REM sleep disorder: A vocal or physical “acting out” of dreams that was not previously present. This can manifest as sleep talking, sudden limb movements, or sleepwalking
- Delusions or visual hallucinations
Advanced Parkinson’s disease dementia
People with advanced Parkinson’s dementia often have severe difficulty moving around by themselves or completing day-to-day tasks. Eventually, people with Parkinson’s dementia may require the use of a wheelchair and around-the-clock care.
People living with dementia and their loved ones should plan for reasonable lifestyle adaptations as the condition progresses.
What causes Parkinson’s disease dementia?
The brain changes in people with Parkinson’s disease are caused by abnormal deposits of a protein (called alpha-synuclein) in the brain. This protein is present in healthy brains, though scientists don't fully understand its normal biological function.
These protein deposits are called “Lewy bodies”, after Frederick H. Lewy, MD., the doctor who first identified them. It’s thought that Lewy bodies effectively leach proteins from healthy brain cells that are necessary for repair. This leads to the progressive nerve cell death seen in Parkinson’s and Parkinson’s disease dementia.
The causes of Parkinson’s disease and Parkinson’s dementia are not fully understood, though various genetic factors are known to play a role.
Risk factors associated with Parkinson’s disease dementia
Doctors have identified several risk factors that may increase a person with Parkinson’s chances of later developing dementia. These include:
- Being male
- Having a family history of dementia
- Being older at the time of onset
- Severe sleepiness during the day
- Hallucinations
- More severe movement symptoms at the time of onset
- Postural Instability and Gait Disturbance (PIGD) - this may present as “freezing” mid-step, difficulting initiating a step, issues with balance, or shuffling
What is the difference between Parkinson’s and Parkinson’s dementia?
Parkinson’s disease - without dementia - primarily affects movement. Parkinson’s dementia is a form of cognitive decline that only people with Parkinson’s can develop. The symptoms of the condition are similar to other forms of cognitive decline, such as Alzheimer’s disease or other types of dementia, but the underlying cause is different.
Are Parkinson’s dementia and Lewy Body dementia the same?
Parkinson’s disease dementia and Lewy Body dementia are closely related conditions. It’s common to hear them both being referred to as “Lewy Body” dementia, as in both conditions Lewy bodies (alpha-synuclein deposits) are present in the brain.
The main difference between the two conditions is the order in which symptoms appear. In Lewy Body dementia, the symptoms of cognitive decline appear first, with movement symptoms presenting later - if they occur at all.
In Parkinson’s dementia, movement symptoms are always present and are the first symptoms to appear; cognitive symptoms develop later.
How is Parkinson’s dementia different from Alzheimer’s disease?
Like Lewy Body dementia, Alzheimer’s disease initially presents with cognitive symptoms.
The early signs of Alzheimer’s disease include:
- Difficulty recalling names and familiar words
- Misplacing objects
- Difficulty performing previously easy tasks (such as making a cup of tea)
- Increased difficulty with organisation
The biological causes of Alzheimer's disease differ from Parkinson's dementia - though there are similarities. In both conditions, protein deposits form in the brain, which impairs brain cell function and speeds up cell death.
However, the type and nature of the protein deposits in a brain affected by Alzheimer’s differ from those seen in Parkinson’s dementia. Those with Alzheimer’s typically present with beta-amyloid “plaques” and clumps of tau proteins known as “neurofibrillary tangles”.
How is Parkinson’s disease dementia diagnosed?
Parkinson’s disease dementia is typically diagnosed when the person with Parkinson’s disease goes to their doctor with symptoms of cognitive decline.
The exact diagnostic process used to identify the condition varies from one case to another. Doctors may employ a range of simple memory and task-based tests to measure the person’s level of cognitive function.
The Montreal Cognitive Assessment (MoCA) is one such test frequently used in the diagnosis of dementia conditions and Alzheimer’s disease. The test takes 10 minutes and assesses short-term recall, orientation, and visuospatial abilities (perception of spatial relationships between objects).
What if motor symptoms and cognitive symptoms occur simultaneously?
There are cases in which a person who has not been diagnosed with Parkinson’s disease presents with cognitive and motor symptoms that have started to occur simultaneously. In these instances, a diagnosis of Lewy Body dementia is more common.
What are the treatments for Parkinson’s dementia?
Parkinson’s dementia is a degenerative condition that cannot be cured and worsens over time. No recognised medical treatments are known to slow the onset of cognitive symptoms.
However, several treatments and therapies are known to ease symptoms and significantly improve the quality of life.
Medication for dementia
Doctors may prescribe medication to help people with Parkinson’s dementia cope with their symptoms.
Commonly prescribed medications include:
- Antipsychotics, antidepressants or neuroleptics: These drugs may be prescribed in very low doses to help with mood swings and other behavioural symptoms.
- Cholinesterase inhibitors: These drugs can help with visual hallucinations, disturbed sleep, clarity of thought and mood problems.
Other treatments and therapies
Many people with Parkinson’s dementia find that physiotherapy and speech therapy can help with symptom management.
Other non-medical forms of therapy may also be beneficial. For instance, music therapy can positively impact mood and support long-term recall in people with dementia.
Caring for a person with Parkinson’s dementia
Caring for a person with Parkinson’s disease dementia can be challenging. This is especially true when the condition is in its advanced stages, as they may begin to show signs of agitation, delusions, or severe mood fluctuations, in addition to their motor symptoms.
Fortunately, there are a few simple strategies you can easily implement to help the person you’re caring for remain calm and happy. For example:
- Stick to routines and develop structured schedules to increase comfort and familiarity
- Choose simple decor that will minimise distraction and promote calm
- Speak calmly, slowly and clearly to minimise anxiety and agitation
- Some people with dementia sleep better with nightlights. You might consider using one if the person you’re caring for experiences delusions or becomes upset during the night
- Be sure to show the person living with dementia that you care and have affection for them. This will reduce feelings of frustration and improve self-worth
- If the person you are caring for becomes aggressive or paranoid towards you, remember that it’s the illness talking - not them
Activities for people with Parkinson’s dementia
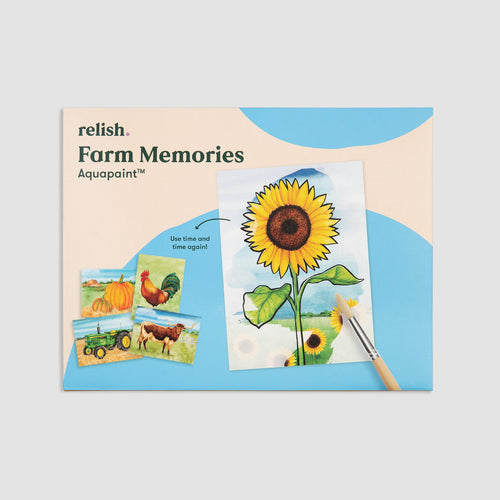
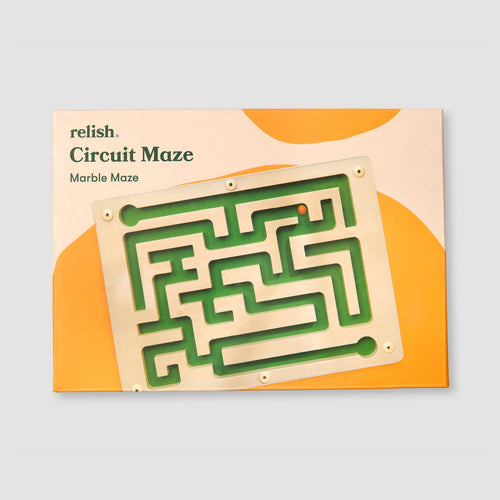
It's essential that people living with dementia have ways to remain mentally active. Some experts believe that stimulation - in the form of games, brainteasers, jigsaw puzzles or arts and crafts - could slow the worsening of symptoms.
In addition, these kinds of activities provide enrichment, allow for interaction with loved ones, and improve quality of life.
Different activities are suitable for different stages of Parkinson’s disease dementia. Find out your stage of dementia and select appropriate activities accordingly.
Learning to live with Parkinson’s disease dementia
A diagnosis of Parkinson’s dementia is never easy. It can be beneficial for all parties involved to understand the nature of the illness, what causes it, and how it is likely to progress.
Knowledge often helps with acceptance and can provide valuable insights into maintaining quality of life as Parkinson’s disease progresses.
At Relish, we believe in helping people with dementia live with joy and connection. We develop dementia-friendly products specifically designed to support better wellbeing and quality of life for those living with dementia. Visit our website for more information on products, activities and support for people living with dementia.