Dementia is a progressive condition that affects memory, thinking, and the ability to manage daily life. While Alzheimer’s disease is the most common type, there are several forms of dementia, and each person’s experience is unique.
Understanding how dementia progresses can help you feel more prepared for the journey ahead. An early diagnosis gives you the chance to make plans, access helpful support services, and focus on what matters most: enjoying the present moment with your loved one.
Although everyone’s path is different, healthcare professionals often describe dementia in stages. These stages can guide you in recognising symptoms, understanding what to expect, and finding the right support along the way.
In this guide, we’ll gently walk through the stages of dementia, explore common signs at each phase, and share tips to help you support someone living with dementia with care and confidence.
Understanding Dementia Staging Models
Dementia doesn’t follow a strict timeline, and symptoms can affect each person differently. However, to help families and caregivers understand what might come next, professionals often use staging models to describe how dementia progresses over time.
To better support those affected, we've identified four key stages of dementia progression:
- Early Stage – Subtle changes in memory and thinking may begin to emerge, often going unnoticed. Individuals might experience minor lapses but can generally maintain independence.
- Early to Mid Stage – Symptoms become more noticeable, with increasing difficulty in managing daily tasks. Support and reminders may be needed to maintain routines and independence.
- Mid to Late Stage – Cognitive decline becomes more pronounced, leading to significant challenges in communication and daily functioning. Increased assistance and supervision are typically required.
-
Late Stage – Individuals may lose the ability to function independently, requiring full-time care. Communication becomes severely limited, and physical abilities may decline.
Each person's journey with dementia is unique, and symptoms may overlap between stages. Understanding these stages can help caregivers and loved ones provide appropriate support and plan for the future.
Another model you might hear about is the Global Deterioration Scale (GDS), which outlines seven clinical stages of cognitive decline. This offers a more detailed breakdown, especially useful in medical settings, but the three-stage model is often easier to follow for families at home.
Whichever model is used, they all share a goal: to offer guidance, anticipate care needs and help you support your loved one with clarity and confidence.
If you or a loved one has been diagnosed with dementia, you may find it helpful to take our short Find Your Stage questionnaire to understand which stage you are currently at.
Early Signs of Dementia
In the early stage of dementia, symptoms can be subtle and are sometimes mistaken for normal signs of ageing. You or a loved one might begin to experience changes in memory, mood or cognitive function, but still manage daily life fairly well. This stage often overlaps with a condition known as mild cognitive impairment (MCI) – a noticeable decline in thinking skills that doesn’t yet interfere significantly with day-to-day living.
Common early symptoms include:
- Repeatedly forgetting recent events or conversations
- Misplacing items like keys or glasses more frequently
- Struggling with problem-solving or complex tasks, such as following a recipe
- Taking longer to find familiar words when speaking
- Feeling overwhelmed by decisions or changes in routine
You might also notice mood changes, such as increased anxiety, irritability or a loss of interest in hobbies. Some people become more withdrawn socially, sensing that something isn’t quite right.
In the early stage of Alzheimer’s, difficulties with cognitive ability may extend to navigation, time management or recognising faces in crowded places. Tasks that were once second nature, like managing finances or remembering appointments, may require reminders or gentle support.
Although these signs can cause concern, they also provide a valuable opportunity. An early diagnosis opens the door to support services, legal and care planning, and lifestyle changes that may help slow the rate of cognitive decline. This stage is also a time to focus on joy, meaningful connection, and living well in the present moment.
For appropriate activities suited to this stage of dementia, see our guide here.
Early to Mid Stages of Dementia
As dementia enters the space between the early and middle stages, symptoms become more noticeable and start to affect daily life in a more consistent way. This is when cognitive changes often shift from mild forgetfulness to more significant challenges with everyday activities and communication.
People in this stage may:
- Struggle to keep track of conversations or follow storylines on TV
- Forget important details such as birthdays or personal history
- Get confused more easily when making decisions or managing time
- Experience difficulty with paying bills, preparing meals, or navigating new environments
This is also when routine tasks, like choosing appropriate clothing, remembering scheduled appointments or preparing food, might need assistance or prompting. While many individuals may still live and function independently, they may become more reliant on others for structure and support.
Changes in cognitive ability can also impact relationships. A person may become quieter, more easily frustrated or anxious in unfamiliar situations. These shifts can be difficult for family members, especially when a loved one begins to withdraw from hobbies or avoids social situations that were once enjoyable.
At this stage, it can be helpful to introduce gentle routines and support tools that reduce stress and promote confidence, such as a dementia reminder clock for task management.
Having familiar objects nearby, simplifying daily choices and encouraging low-pressure activities can all make a meaningful difference. If you haven’t already, this may also be the right time to start exploring in-home care, dementia-friendly products and activities for early-mid stage dementia and local support groups.
Mid to Late Stages of Dementia
In the middle to late stages of dementia, symptoms become more advanced and start to affect both mental and physical abilities. Support is often needed not just occasionally, but consistently, as changes in memory, behaviour and communication become more pronounced.
At this stage, memory problems may extend to forgetting the names of close family members or confusing them with others from the past. People may have difficulty speaking in full sentences or may lose their train of thought midway through a conversation. Repeating questions, getting lost in familiar places and forgetting daily living routines like bathing or dressing are common.
You may also see:
- Mood swings or emotional outbursts
- Increased trouble controlling impulses or behaviour
- Disrupted sleep patterns or nighttime wandering
- Changes in motor skills, such as difficulty walking or balancing
These changes can be distressing, but they’re not intentional. They stem from the brain’s gradual loss of ability to process information, manage emotions and respond appropriately. As cognitive ability declines, so too does the ability to reason or make sense of surroundings.
Caregivers often find this period challenging, especially as a loved one may struggle to recognise familiar faces or may feel frightened and disoriented. Creating a calm, structured environment and using reassuring language can help reduce agitation. Home aids, soothing mid–late stage activities like music and familiar scents or objects can be powerful tools for comfort.
Although independence is reduced, many people at this stage can still enjoy shared experiences, listening to a favourite song, looking through photo albums or feeling the warmth of a familiar hand.
Similarly, caregivers might find it helpful to read this article on coping with the behavioural changes dementia brings.
Late Stages of Dementia
In the final stage of dementia, also known as severe or advanced dementia, a person will often need full-time care and support. As the condition reaches this point, both cognitive function and physical abilities decline significantly, and the person may no longer be able to communicate their needs or function independently.
Common signs at this stage include:
- An inability to recognise even close loved ones
- Limited or no speech due to loss of language skills
- Difficulty swallowing and a higher risk of choking or weight loss
- Incontinence and trouble controlling bowel and bladder functions
- Stiffness in the limbs, loss of balance or inability to control movement
- Increased sleeping and reduced responsiveness
These changes reflect the breakdown of brain cells and nerve cells, especially in the areas of the brain responsible for motor skills, memory and language. A person may also appear unaware of their surroundings or unable to engage in the outside world in typical ways.
While this stage is deeply challenging for families, it’s still possible to create moments of comfort and connection. People in the late stage of dementia often respond to sensory experiences, such as music, scent, soft textures, or gentle hand massage, even when words are no longer accessible. These small, meaningful gestures can help a person living with dementia feel secure and cared for. You might also find inspiration from activity suggestions designed specifically for this stage, which focus on gentle engagement and comfort.
Palliative care and hospice services may be introduced during this time to ensure that the individual remains comfortable, supported and treated with dignity. Though the journey is nearing its end, love, presence and compassionate touch still matter profoundly.
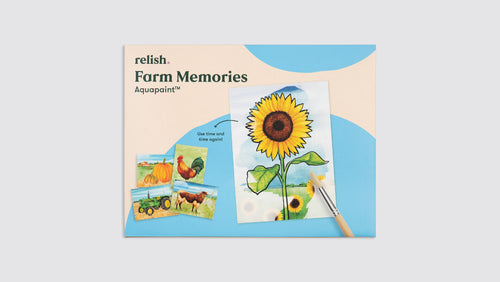
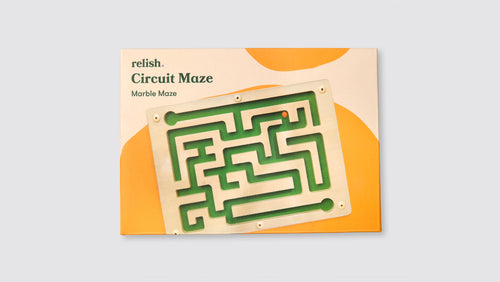
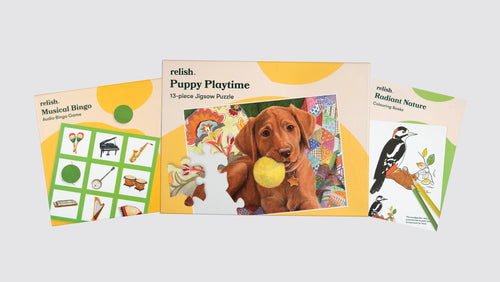
At Relish, we provide a range of soothing products for people in the late stages of dementia.
Take our quick Find Your Stage questionnaire to understand which stage of dementia you or a loved one is at.
Types of Dementia and How They Progress Differently
Although Alzheimer’s disease is the most common cause of dementia, there are several other types, each with its own pattern of symptoms and progression. Understanding the differences can help explain why symptoms vary so much from person to person.
Alzheimer’s Disease
This is the most well-known type of dementia. It typically begins with memory loss and difficulty finding words, gradually affecting problem-solving, decision-making and eventually daily living skills. The progression tends to be slow and steady over time.
Vascular Dementia
Caused by reduced blood flow to the brain, often following a stroke or due to high blood pressure or heart disease, vascular dementia may progress in noticeable steps rather than gradually. Symptoms can include difficulty with concentration, decision-making and physical coordination.
Lewy Body Dementia
This type involves abnormal protein deposits called Lewy bodies that disrupt brain function. People with Lewy body dementia may experience early hallucinations, daytime sleepiness, fluctuations in alertness and movement issues similar to Parkinson’s disease. These symptoms vary from day to day, often making it harder to predict progression.
Frontotemporal Dementia (FTD)
Frontotemporal dementia usually affects younger individuals and targets the parts of the brain responsible for behaviour and language. It often begins with significant personality changes, poor judgment or socially inappropriate behaviour, rather than memory issues. Speech difficulties are also common.
Mixed Dementia
Some individuals develop more than one type, most commonly Alzheimer’s disease and vascular dementia, which is known as mixed dementia. This can lead to a broader range of symptoms and a more unpredictable rate of decline.
Get a more in-depth look at the different types of dementia here.
Legal and Financial Planning
The early stage of dementia offers a valuable opportunity to plan ahead, before cognitive functioning declines further. While it can be difficult to think about the future in these terms, making legal and financial decisions early can reduce stress for both the person living with dementia and their family members.
One of the most important steps is setting up a lasting power of attorney. This allows a trusted person to make decisions on behalf of the individual with dementia when they’re no longer able to do so themselves.
It’s also a good time to:
- Create or update a will
- Establish advance care directives
- Outline personal wishes for future medical treatment and living arrangements
Financially, it’s helpful to simplify accounts, set up automatic bill payments and appoint someone to assist with managing expenses. These steps protect the person’s independence and safety while ensuring that their affairs remain in order as daily life becomes more challenging.
Having these conversations early means decisions are made with the person’s full input, reflecting their values and preferences, not just practical needs. While every situation is unique, proactive planning can ease the journey for everyone involved and help maintain dignity throughout the stages of dementia.
Diagnosis and Assessment
Recognising the early signs of dementia is an important first step, but getting a clear and timely diagnosis is equally vital. An early diagnosis can open the door to helpful support services, allow for thoughtful planning and provide clarity for both the person experiencing changes and their loved ones.
Diagnosis usually begins with a visit to a GP, who may carry out simple memory checks and talk through any noticeable changes in daily life. They’ll ask about difficulties with recent events, handling complex tasks, or whether the person is struggling to find the right words. From there, they may refer the individual to a specialist or a memory clinic for further assessment.
At this stage, doctors may use questionnaires or brain imaging to look at changes in cognitive functioning and determine whether symptoms fall within recognised clinical stages – from mild cognitive impairment to more advanced dementia.
Tracking a person’s cognitive decline helps to understand how best to support them, and what kinds of care, therapies or activities might help. Organisations like Alzheimer’s Society and local dementia support groups can also guide families through the diagnostic process and what comes next.
Lifestyle Tips for Slowing Progression
While there is no cure for dementia, research shows that certain lifestyle choices may help support brain function and potentially slow the progression of the condition. These small, everyday habits can make a meaningful difference, especially in the early stages of dementia or even before symptoms begin in people at risk of developing dementia.
Here are a few evidence-backed tips that may help:
- Stay physically active – Walking, gentle stretching, or chair exercises help increase blood flow to the brain and support overall wellbeing.
- Eat a balanced diet – Foods rich in antioxidants, healthy fats and leafy greens can be beneficial for brain health. Managing high blood pressure and avoiding excess sugar or processed foods is also important.
- Stimulate the mind – Activities like puzzles, games, reading and reminiscence therapy help keep the brain engaged and may slow cognitive decline.
- Stay socially connected – Talking with friends, joining a club, or even short daily chats can reduce loneliness and support emotional health.
-
Manage underlying conditions – Treating things like heart disease, diabetes and sleep problems can protect overall health and reduce added strain on the brain.
Equally important is the reminder to embrace the present moment. Whether it’s enjoying a favourite song, sharing a cup of tea or spending quiet time together, simple experiences can offer joy and connection, no matter the stage of dementia.
FAQs About the Stages of Dementia
What are the early symptoms of dementia?
Early symptoms can vary from person to person but often include memory loss, trouble with problem solving, forgetting recent events or struggling to find familiar words. These signs may be subtle at first and are sometimes mistaken for normal ageing. If you’re concerned, an early diagnosis can help clarify what’s happening and open up support options.
How quickly does dementia progress?
The speed at which dementia progresses depends on the type of dementia, the person’s age, overall health and other factors. Some people experience a gradual decline over many years, while others progress more quickly. On average, the early stage may last around two years, the middle stage around two to four years, and the late stage dementia one to two years.
What affects life expectancy after a dementia diagnosis?
Life expectancy can vary widely. It often depends on when the dementia was diagnosed, how well other health conditions are managed (like heart disease or high blood pressure), and the person’s resilience and support system. Staying socially active, eating well and managing stress can all play a role in living well for longer.
How are the clinical stages of dementia diagnosed?
Doctors may use a combination of cognitive tests, medical history and scans to understand a person’s cognitive decline. They might refer to clinical stages like the Global Deterioration Scale to describe how far the condition has progressed. These assessments are useful for planning care and tracking changes over time.
When is it time to consider care support?
If someone is struggling to perform routine tasks or stay safe at home, or their care needs are becoming overwhelming for loved ones, it may be time to explore additional help. This could mean arranging in-home care or considering a care home, depending on what feels right for your situation.
Improving Wellbeing For People Living With Dementia
At Relish, our mission is to bring joy and ease into daily life for people with dementia and their caregivers. If you’re not sure what stage your loved one is at, our short questionnaire can help point you in the right direction and guide you to dementia-friendly products suited to their needs.
Gain free access to our bank of 100+ dementia activities by simply signing up with your email.